Type 1 Diabetes Care Directive
People with Type 1 Diabetes know their care better than anyone because they live with it and manage it daily. Some HCPs' training in T1D is not up to date. Some do not perform patient-centered care. PWT1D receives low-quality care or are not satisfied with the care they received.
As a solution, we designed T1D Care Directive, a lightweight tool that promotes shared decision-making. A more elaborate version is on the way.
Role
Product Designer, UX Researcher
Duration
June 2021, 20 weeks
Team
Jodie Li, Jhea Espares, Denise Tang
Overview
Given our understanding of the problem spaces through our prior need-finding research, we narrowed the focus onto the need to bridge the gap between people with type 1 diabetes and healthcare providers. We focused on answering:
“How might we design a new tool for two distinct types of users (people with type 1 diabetes and health care workers) such that quality of care can be improved through shared-decision making?”
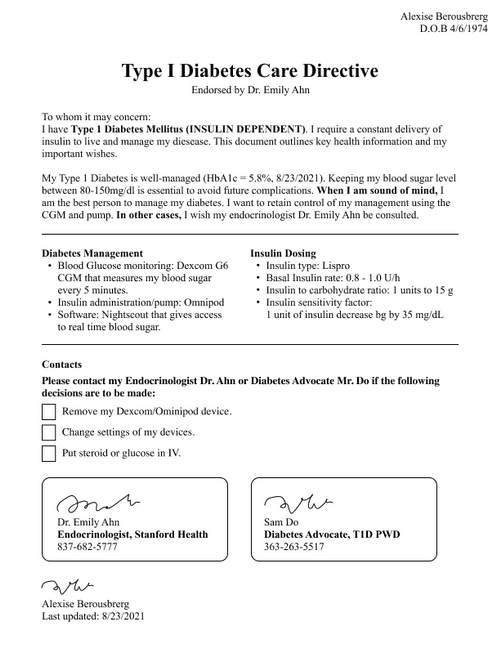
While there are care plans and advance care planning and advance directives available to people, to our knowledge, there is not a “living directive designed for people living with diabetes. Therefore, we propose a “T1D care directive” that could be useful to aid people with type 1 diabetes.
- In total, I conducted 7 user interviews and 10 usability tests (doctors and PWT1D) in this project cycle.
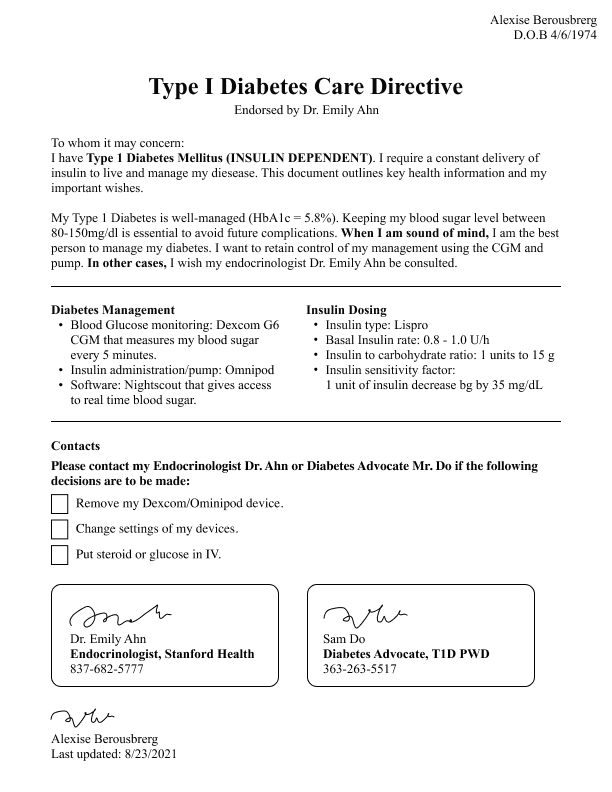
- I created the MVP of the type 1 care directive.
- I created the product website to improve the onboarding experience of the product.
1. Document Ideation
2. Website Design
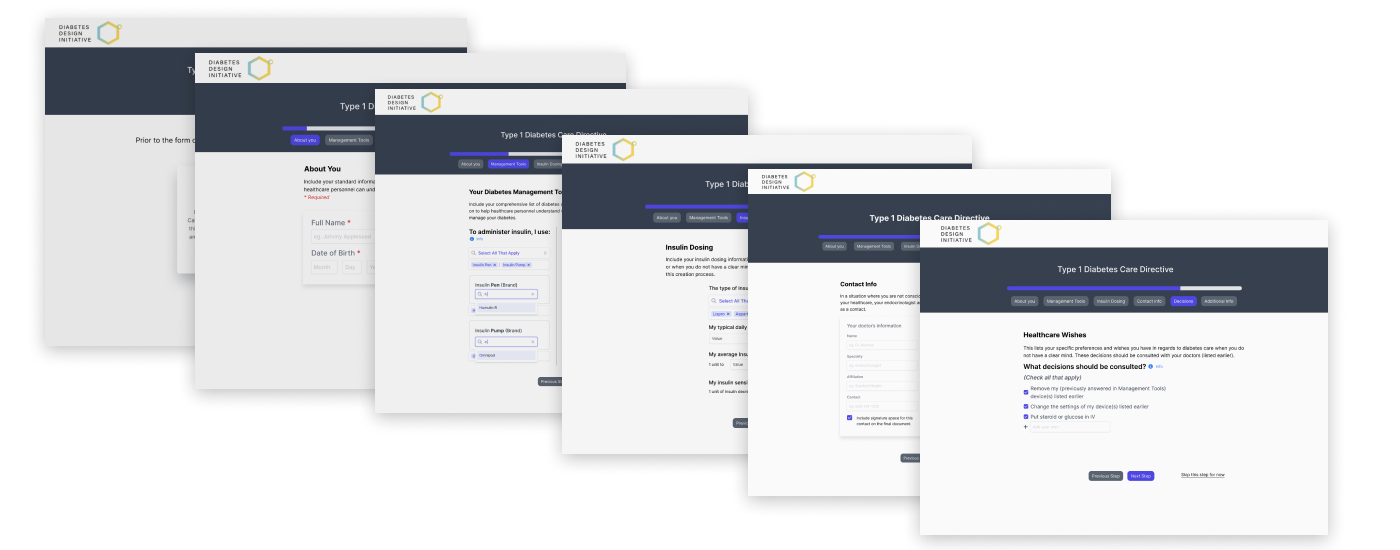
3. Form Filling Design
Research
We conducted several rounds of user interviews on Zoom over three months asking questions about their experience with healthcare providers, from nurses to endocrinologists, to challenge our assumptions and refine our design direction. We chose to use an affinity map, a similar design artifact as mindmaps, to visually analyze our findings into patterns and themes.
In total, we conducted 10 user interviews: 6 PWD, 3 HCP, and 1 PWD who is an HCP themself. We asked questions including, but not limited to, the relationship between PWD and HCP, conflicts PWD had experienced, struggles of being an aging PWD, and a possible medical resume/directive.
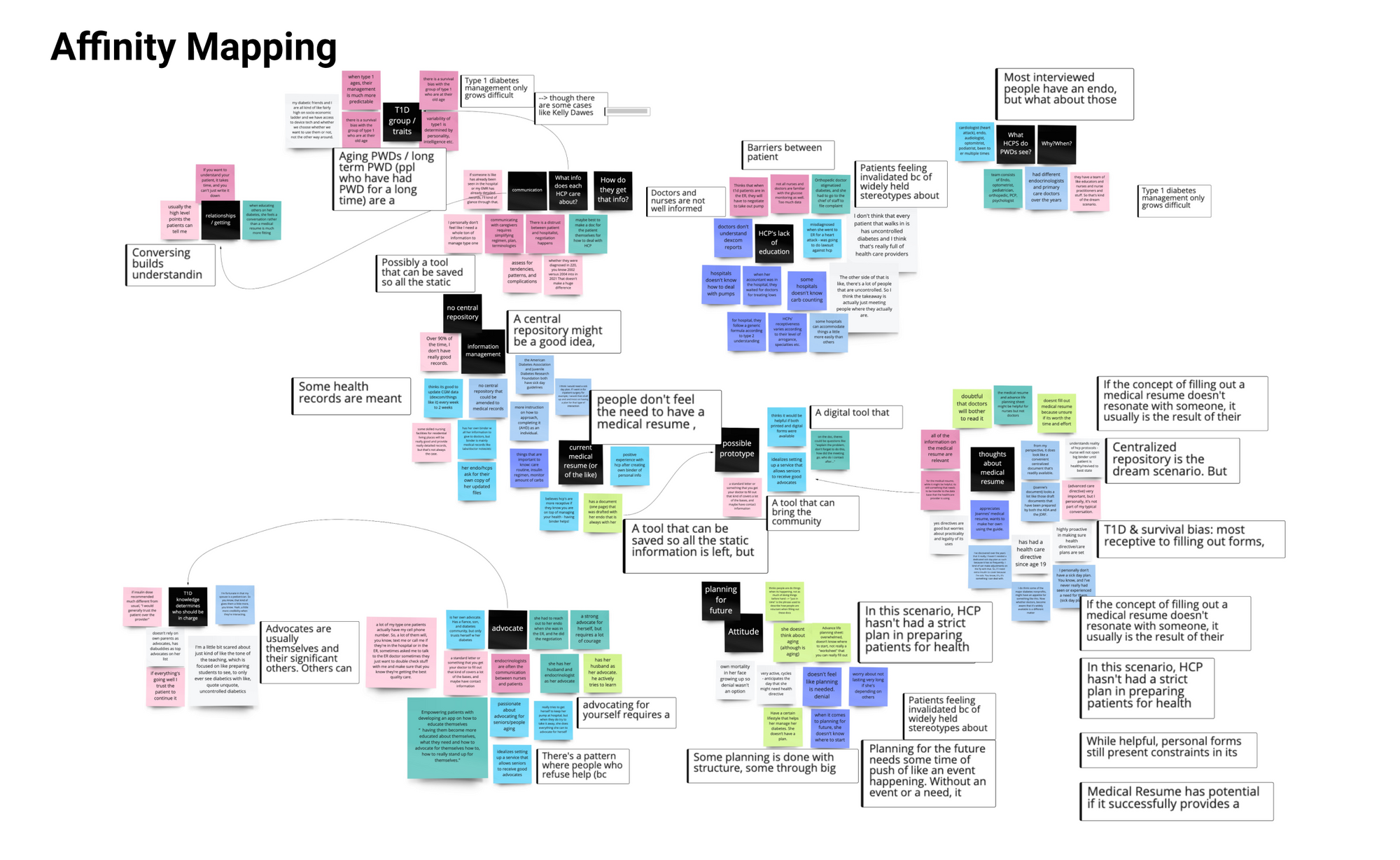
Interview Insights
1. PWT1D who are motivated to plan for the future experienced landmark events that get them out of denial of death.
- Without life changes/landmark events that act as a catalyst, the sense of denial often becomes the blocker that prevents individuals from planning ahead.
- One's cultural worldview and self-esteem (confidence in one's own abilities to live a full life) also play a role in taking steps to plan for the future. (Terror Management Theory
2. Trust and understanding between PWD and HCP stem from having meaningful conversations.
- However, communication is prevented by strict hospital protocols and HCP having stereotypes of PWD having uncontrolled diabetes and not taking good care of themselves.
- HCP’s assumptions about HCPs (they will ignore medical resumes) based on disappointing past experience reduces the willingness to fill out a medical resume/external tools.
With these insights, we learned that being overly prepared and involved in their health management and progress greatly improves the quality of care patients receive from their HCPs. Trust, here, is built on both ends. How might we bring empowerment into the hands of T1D so that they have the means to build this trust?
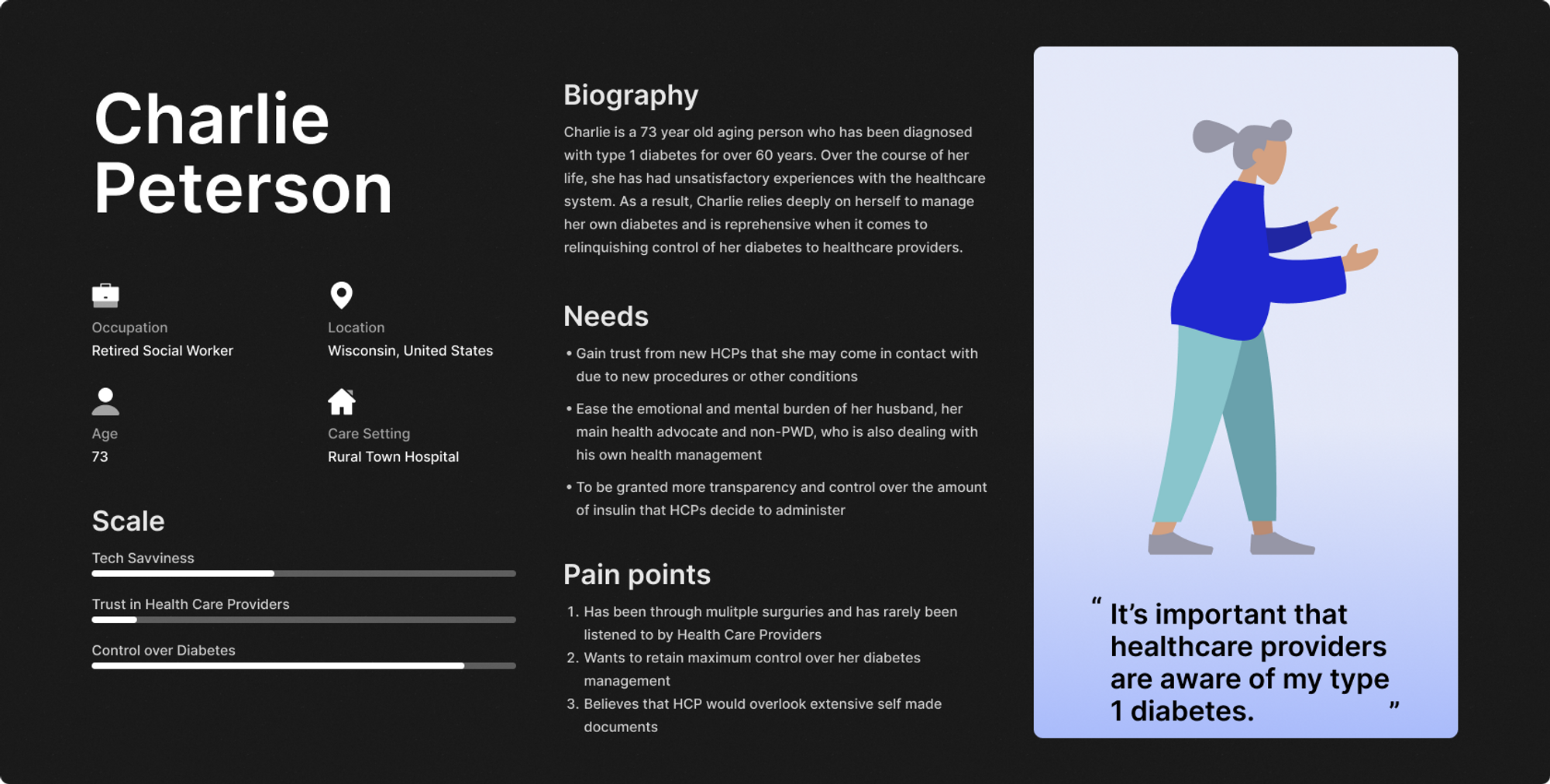
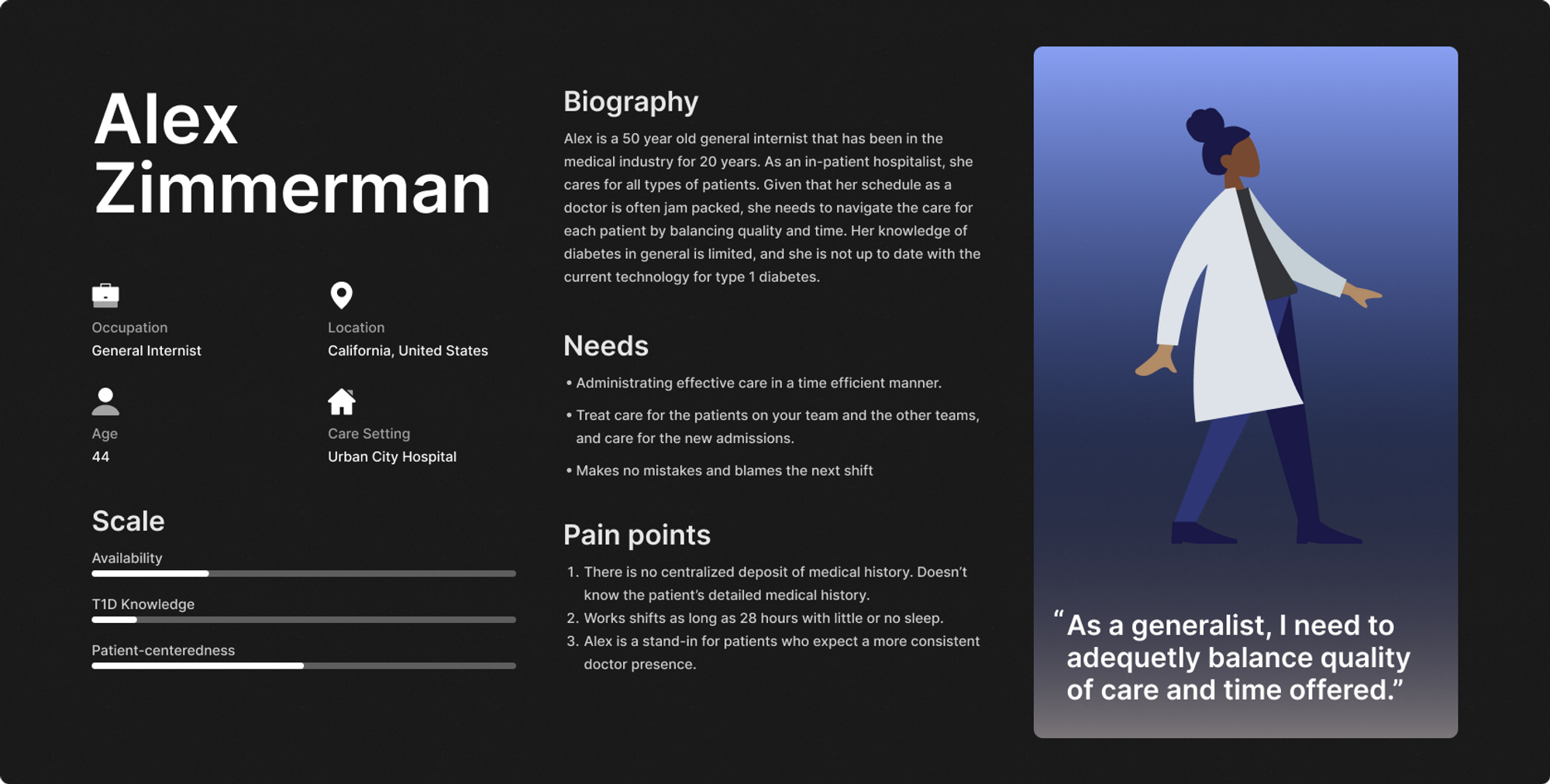
Personas - Summarizing Interviews
Personas are abstractions of our target users based on our research. Our target users are PWDs and HCPs. By creating these abstractions, we aimed to understand the varying and similar contexts and needs of our two target user groups.
We wanted to lay out the general issues both sides have regarding their interactions, whether it be troubled perception or a lack of resources. Some of the main findings we wanted to reflect into these personas are the desire for PWD to be given transparency over diabetic management by HCPs, and the importance of time for busy HCPs.
Design
We decided to design a tool that will help T1D improve their healthcare experience. After several rounds of brainstorming, we decided to move forward with a “Type 1 Diabetes Directive”.
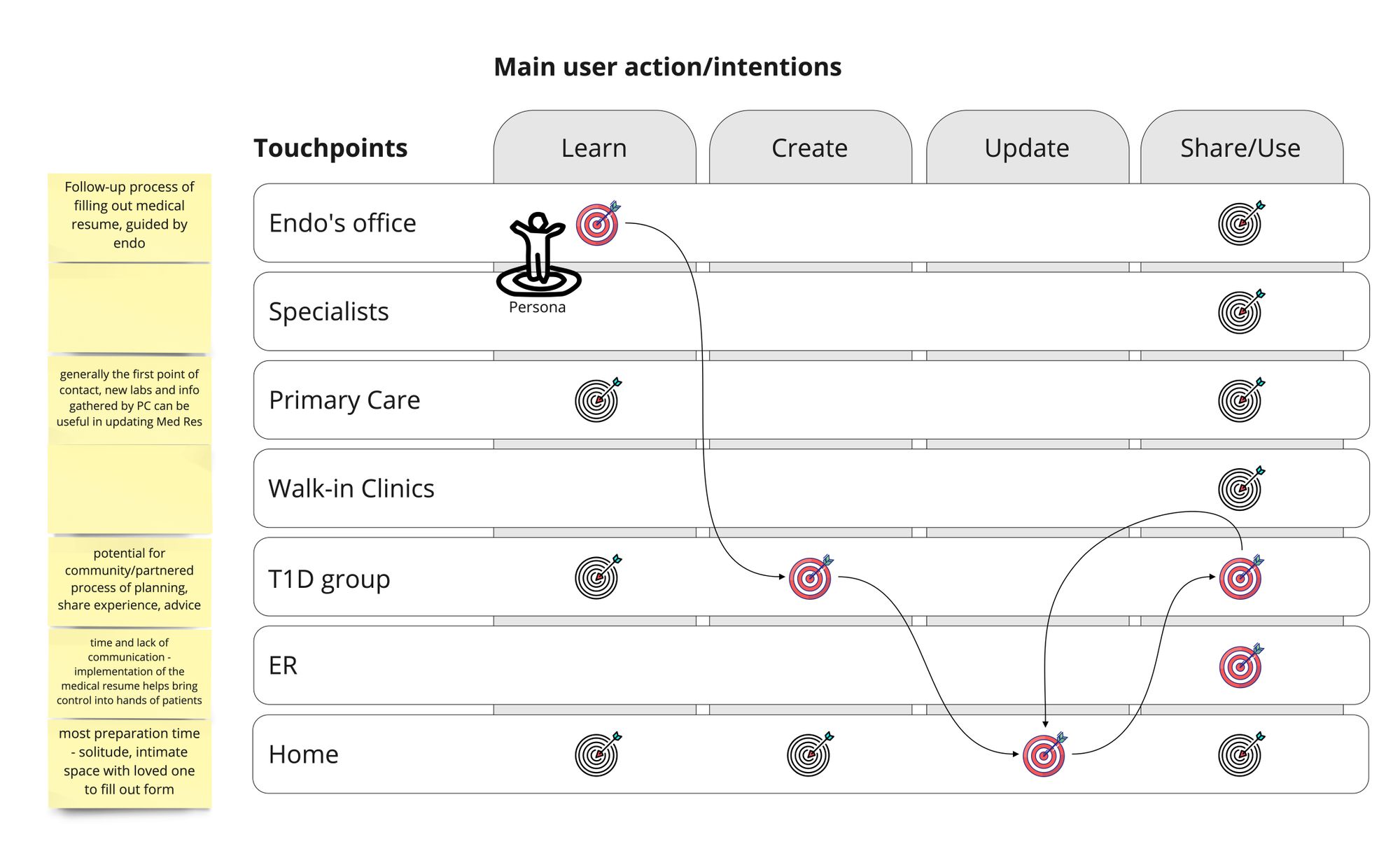
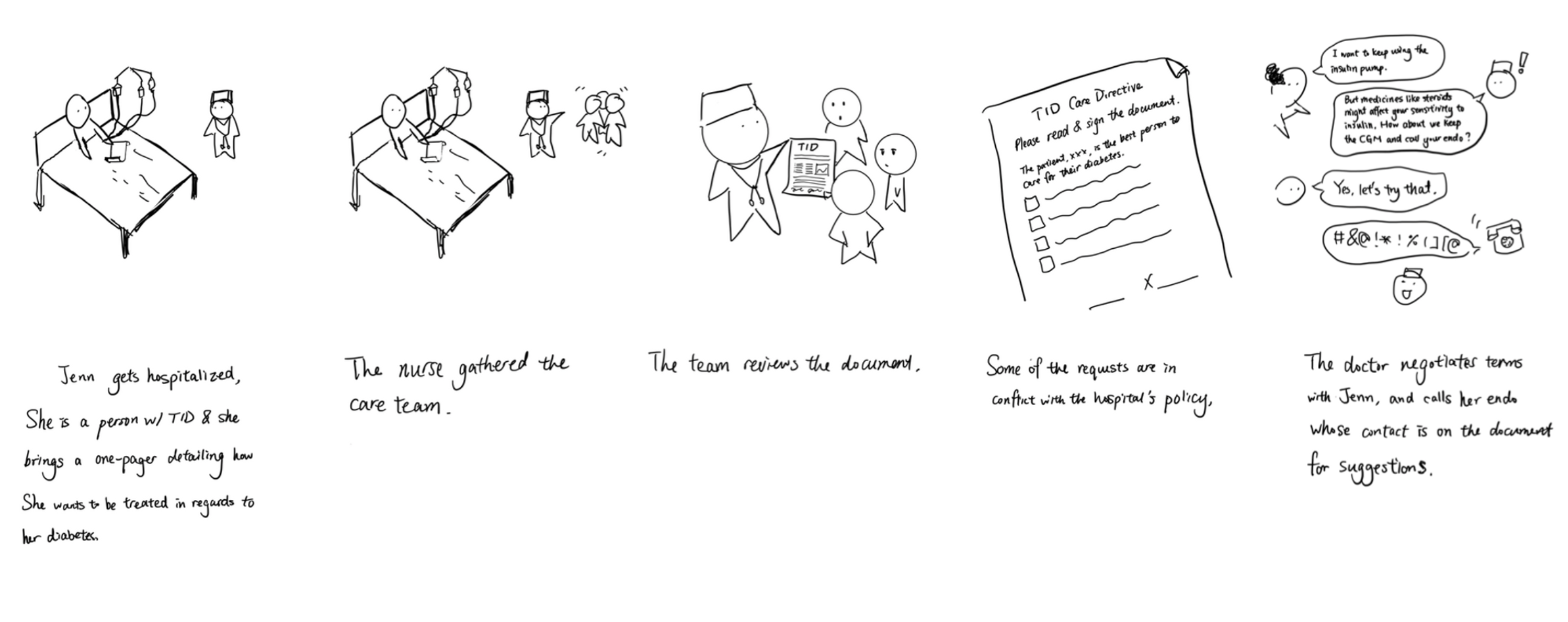
Visualizing the Experience
This storyboard shows how it is used:
This experience map shows the scenarios and process related to creating and using the directive:
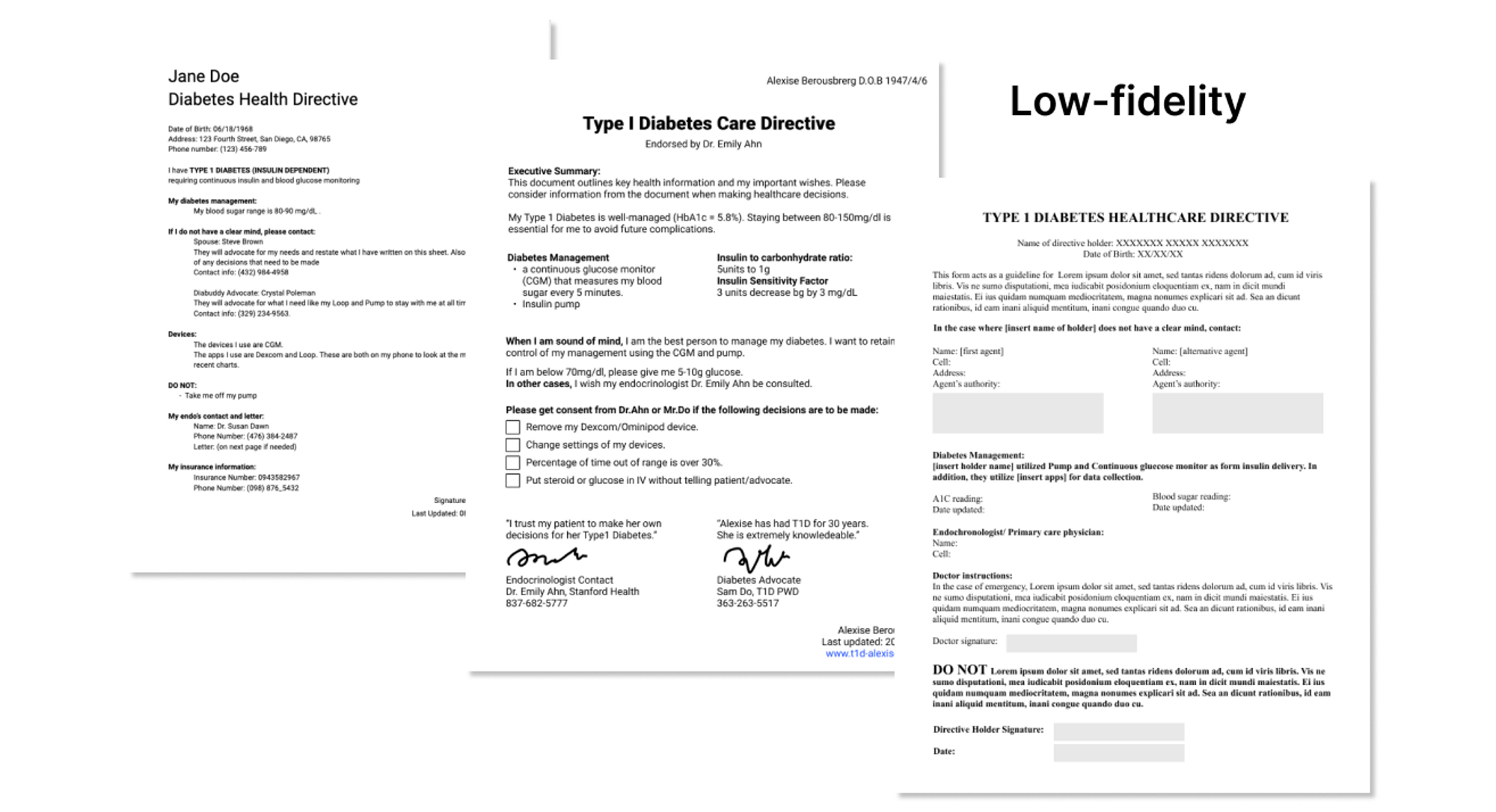
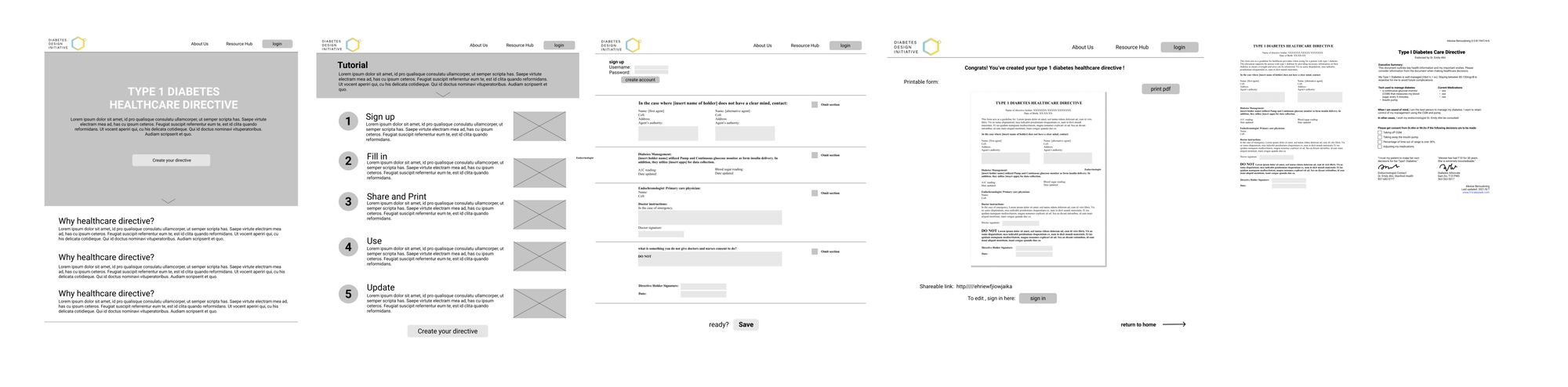
Wireframing
Our team developed a wireframe and lo-fi of the diabetes health directive. Using our information from our user insights and learnings, we each put together a wireframe, and merged parts of each one into a single page that we could show for another round of interviews.
We wanted this to be specifically short, considering that some PWD assumed that a long directive would deter HCP from reading it. Also, brief information about their management shows some credibility of being in charge and control of their diabetes. At the bottom, we included statements of PWD needs and the people they depend on if their needs cannot be met. We considered it would be important for negotiation by bringing in a medical professional like an endocrinologist.
User Testing
We interviewed a total 6 healthcare providers, including doctors from UC San Diego Health and Stanford Health, and conducted usability tests through story board and A/B testing. The result shows that a short directive is valuable in certain settings where HCPs might not have sufficient knowledge on type 1 diabetes.
Some concepts we tried to validate are:
- Length: Longer vs. shorter
- Tone: Formal vs. personal
- Hierarchy: express with layout vs. highlighting
- Expertise: prove with knowledge and data vs. endorsement
- Care details: list what to do vs. what not to do
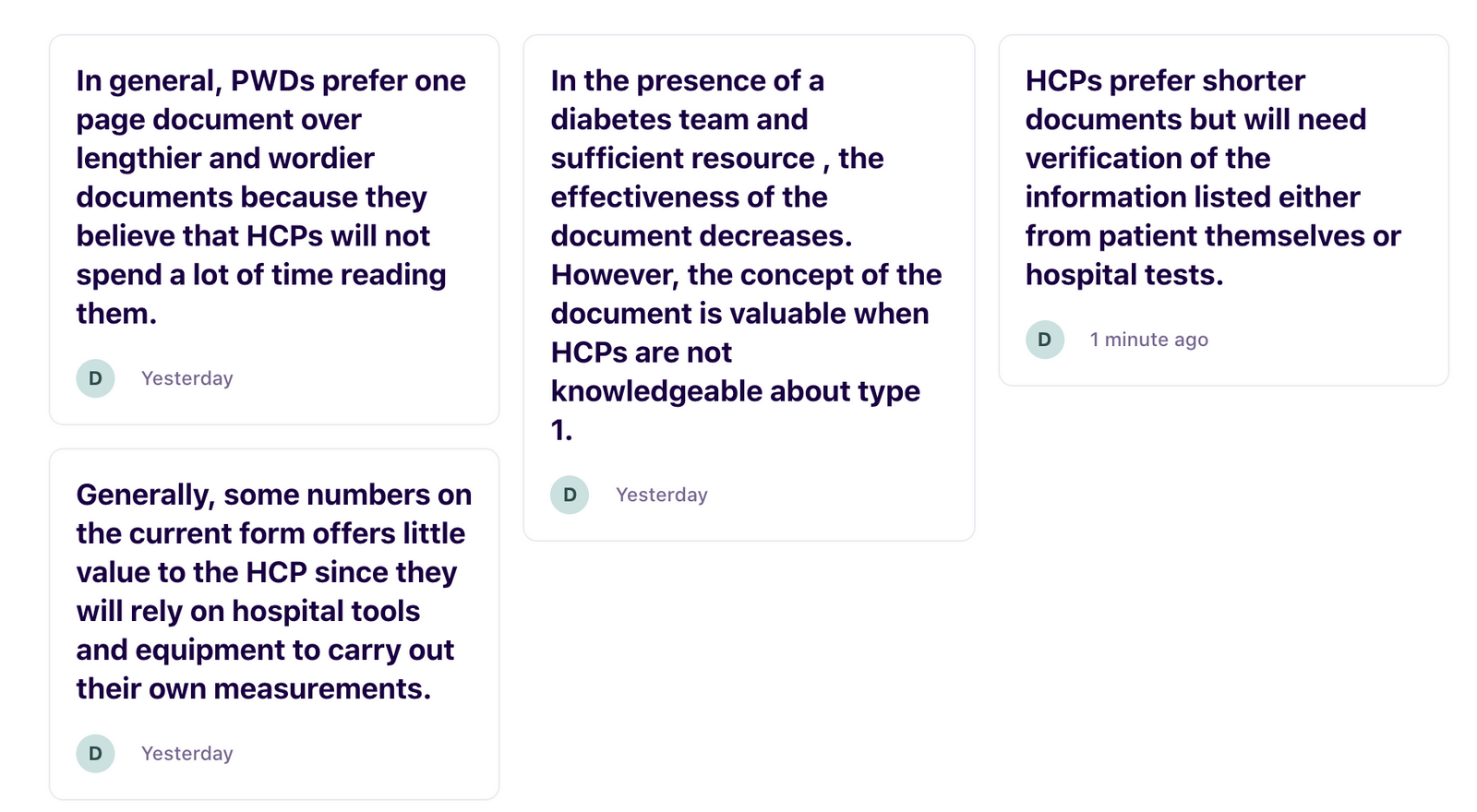
User Testing Results
Based on the usability testing, we were able to identify important insights in regards to the directive.
1. People with Type 1 diabetes believed that a shorter version of the form would lead to a higher chance of success in terms of garnering attention from Healthcare providers.
- This was an assumption that was supported by past experiences of PWDs where they encountered HCPs who were not receptive to what the PWD had to say.
- 5/5 users in the usability testing interview expressed similar opinions on the length of the document.
2. Healthcare providers prefer shorter documents but will need verification of the information listed either from patients themselves or hospital tests/records.
- Our usability tests with HCP showed that in-patient doctors were accepting of external documents like that of the Diabetes Care directive.
- However, the form acts merely as a descriptive document and requires verification of information through either the hospital themselves or cross-examination with other official documents.
- 2 out of 3 Healthcare providers that we have interviewed mentioned the need for verification.
3. The effectiveness of the document depends on both the doctor, the staff, and the hospital. In the presence of a diabetes team and sufficient resources, the effectiveness of the document could decrease. However, the concept of the document is valuable when HCPs are not knowledgeable about type 1.
- While one HCP mentioned that the form might not be helpful in the context of their hospital given that they have an internal information storage system that also stores PWD diabetes information, another HCP mentioned that the document would be helpful in scenarios even with sufficient resources (diabetes care team) since the document allows PWD to effectively communicate their concerns.
- This act creates an environment where a patient can feel included in their care through transparency and clear documentation of their needs.
- Although a constraint that patients have to deal with is hospital protocol which may still override the requests of a patient. This constraint exists even when we remove the presence of self-made documents in a care setting, as it affects all patients and is a part of the greater institutional powers of hospital care.
- This act creates an environment where a patient can feel included in their care through transparency and clear documentation of their needs.
4. While the form cannot guarantee that all wishes of the patient are fulfilled by the healthcare providers, it is effective in increasing the credibility of the patient.
- “Having the signatures there, those two signatures is probably more important than the things above diabetes management” - PWD
- “somebody going to take me seriously if I print this out on my printer and take it to the hospital and say, these are my instructions. And as opposed to, this is how best to take care of me.” - PWD
- “So I liked the title just as quick, just kind of to say what this is, type one diabetes chair directive, and that I think really important to have it endorsed by the provider just to lend sort of credence to it” - HCP
Final Design
Website Design Features
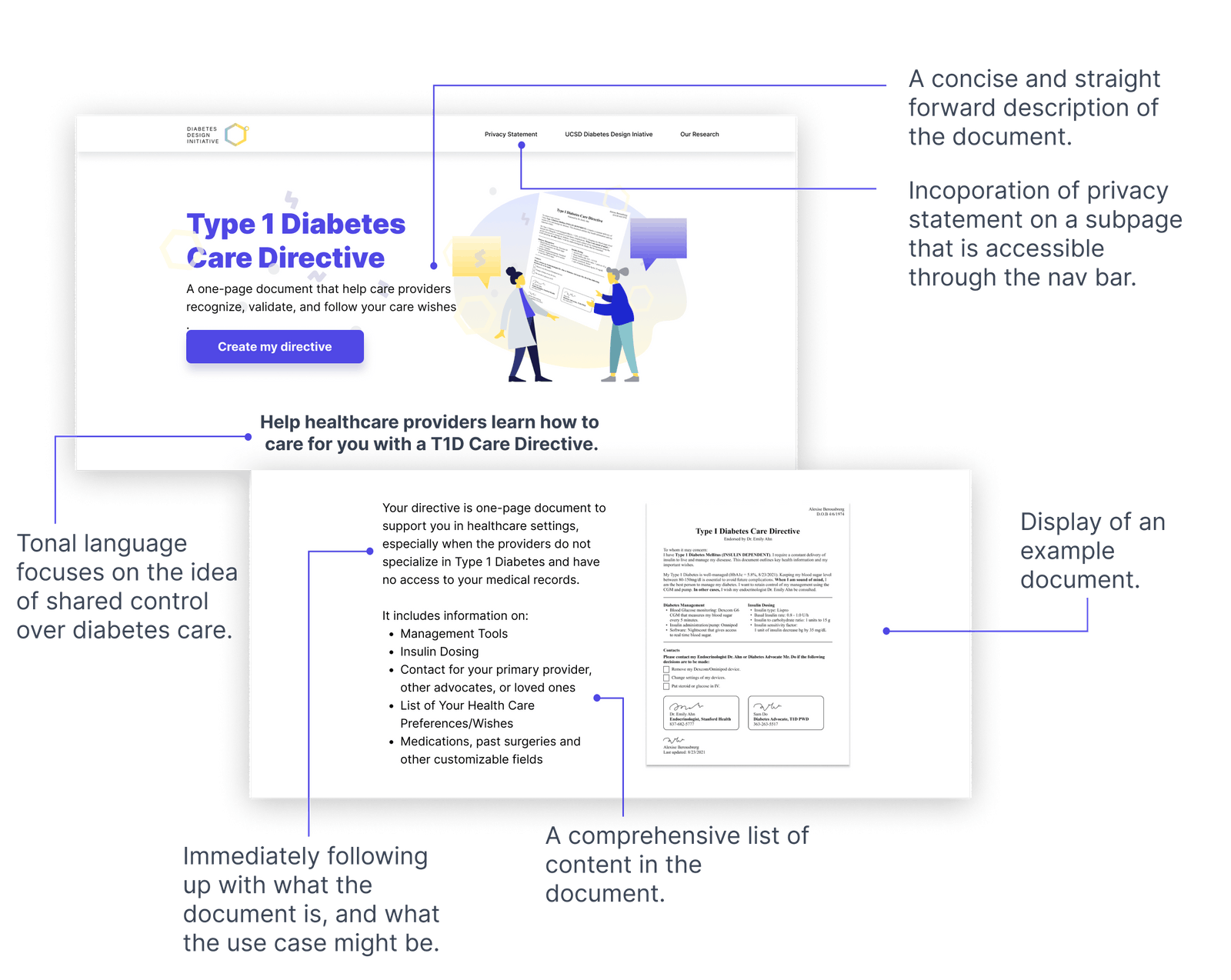
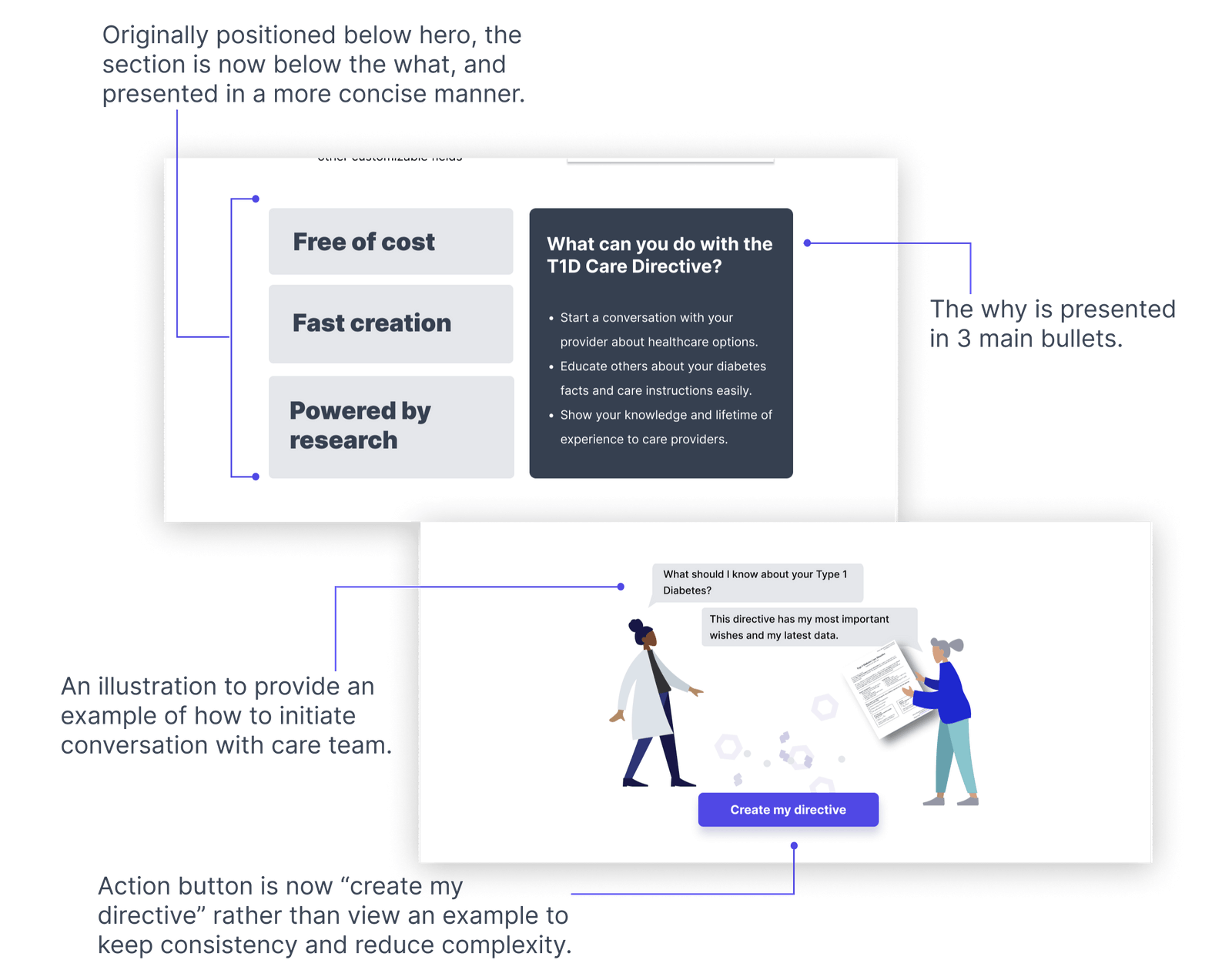
Final Website
Conclusion
Next Steps
Currently, our team is continuing the development of the product as well as seeking partnerships with other research groups and hospitals. Our next steps aim to solidify the implementation plan for our care directive and begin the process of creating a long-term functional platform for people with type 1 diabetes to utilize.
We aim to conduct beta tests with the care directive in a real-life hospital setting to determine the effectiveness of the document and the possibilities for improvement.
Though we are confident in our design of the care directive, we recognized that the artifact itself is only one part of the experience. The process from learning about the care directive, to creating one's own, to updating the document are all steps that must be explored in our next steps. Ultimately, we aim to develop a functioning tool and system.
Takeaways
There are a lot of logistics of designing for health care that needs to be considered, which brings a lot of difficulties. This was a big learning experience for me, where I had to look at the bigger picture with politically and what is implemented in such a vast existing system.
Also, given limited resources, we could not ship and test a beta version of our website prototype. Even with the handoff to developers, there was a lack of being able to bring this to fruition past a Figma design.